PHYSIOTHERAPY IN HAEMOPHILIA MANAGEMENT
- rebounds physiotherapy clinic
- Apr 27, 2023
- 6 min read
Hemophilia is the most commonly known hemorrhagic disorder causing bleeding due to defects in the coagulation factors.
This leads to delay in the coagulation process post injury.
Hemophilia is usually an X linked recessive inherited disease, but in some rare conditions, it has been found to be acquired.

Comparison between types of hemophilia
Haemophilia A
Known as Classical / Standard haemophilia
Protein factor affected Factor VIII
Genetic Inheritance X linked recessive
Gender Affected Mostly males
Acquired haemophilia is rare and occurs as the result of an autoimmune disease that attacks the protein clotting factors (especially factor VIII) and subsequently leads to manifestations similar to haemophilia A.
Haemophilia B
Known as Christmas hemophilia
Protein factor affected Factor IX
Genetic Inheritance X linked recessive
Gender Affected Mostly males
The Royal Disease
Haemophilia C
Known as Rosenthal’s disease
Protein factor affected Factor XI
Genetic Inheritance Autosomal recessive
Gender AffectedFemales & males equally
Manifestations of Haemophilia
Mouth bleeding post-dental extraction or cut.
Nose bleedings
Un-stoppable haemorrhage after a small injury or cut
Blood in urine and stool due to haemorrhage in the kidney / bladder/ intestines or stomach
Haematoma
Joint Bleeding
Muscle Bleeding
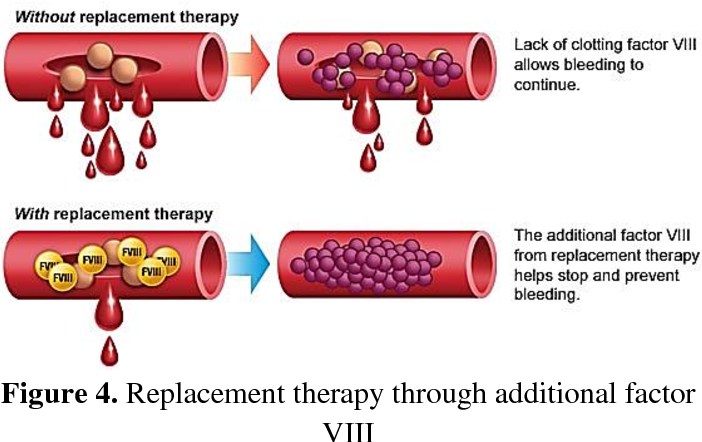
Medical Management
Replacement Therapy : Concentrates of clotting factor VIII (for haemophilia A) or clotting factor IX (for haemophilia B) are slowly injected into a vein to replace the missed clotting factor. These concentrates can be extracted from human blood or synthesized (recombinant clotting factor)
Preventative (prophylactic) therapy
Demand therapy
Physical Therapy In Haemophilia
The National hemophilia Foundation formed a physical therapy working group that created the best physical therapy practice for bleeding disorders including hemophilia.
Role Of Physiotherapy
Reducing the bleeding episodes
Preventing the complications
Improving the quality of life in chronic complications
Rehabilitating patients with severe complications of heamophilia
Joints that have recurrent bleedings in hemophilia are known as “Target Joints”. The most common target joints are knee, elbow, ankle, hip and shoulders
Bleeding into joints and muscles triggering a degenerative process characterized by changes to articular cartilage and other joint structures is the predominant clinical characteristic of haemophilia.
End-stage clinical changes include
reduced joint range of motion (ROM),
flexion contracture,
pain and swelling along with imaging indicators of hemosiderin deposits, synovial hypertrophy,
cartilage and bone erosion.
Prevention of arthropathy is therefore the primary goal of haemophilia treatment.
In countries where prophylaxis is common place, the ankle joint appears the most common site of joint bleeding, whereas, the knee joint is more common when access to prophylaxis is not routine.
For individuals receiving prophylaxis, trauma is often the cause of bleeding, whereas in those receiving on-demand treatments, spontaneous and traumatic bleeds are common.
Rehabilitation goals include achieving prevention and slowing the rate of functional loss, improving or restoring function, compensation for lost function and maintaining current function.
How can musculoskeletal bleeding be
differentiated from arthropathy and other
musculoskeletal disorders?
the early signs of bleeding as a sensation of fullness, stiffness, discomfort, pain or tingling at end ROM but with minimal restriction of movement, and often difficult to distinguish from arthritic pain.
Moderate bleeding is characterized by increased pain, some swelling and restriction of mov9((ement
with severe bleeding, pain is severe, accompanied by marked swelling and almost complete restriction of movement, in other words a ‘joint immobilizing bleed’
PHYSIOTHERAPY IN HAEMOPHILIC –EVIDENCES FOR EFFECTIVENESS
Physiotherapy prevents recurrents Bleeding episodes
(K. Hill, M. Fearn, S. Williams et al., “Effectiveness of a balance training home exercise programme for adults with haemophilia: a pilot study,” Haemophilia, vol. 16, no. 1, pp. 162–169, 2010.
T. Hilberg, M. Hersbsleb, C. Puta, H. H. W. Gabriel, and W. Schramm, “Physical training increases isometric muscular strength and proprioceptive performance in haemophilic subjects,” Haemophilia, vol. 9, no. 1, pp. 86–93, 2003.)
Development of arthropathy affects the proprioception of patients with haemophilia After the treatments described in the studies, proprioception improves as a result of strength and proprioception training programmes for the lower limbs
(T. Hilberg, M. Hersbsleb, C. Puta, H. H. W. Gabriel, and W. Schramm, “Physical training increases isometric muscular strength and proprioceptive performance in haemophilic subjects,” Haemophilia, vol. 9, no. 1, pp. 86–93, 2003)
Points To Remember
Risk Of Anaemia
Risk Of Bleeding
Lack Of Joint Proprioception
Proper Hydration Level
PHYSIOTHERAPY IN HAEOPHILIA- CONDITION WISE
Muscle Reactions to Bleeding
Muscles that react by tightening include the flexor muscles of the wrist and fingers, calf muscles, hamstrings, and hip flexor muscles (iliopsoas).
Muscles that react by weakening include the quadriceps, triceps, and hip extensor muscles. Over time, the weak muscles become weaker and the tight muscles become tighter.
Iliopsoas Muscle Bleeding
Muscle bleeds are the second most common sites of bleeding in haemophilia (after joint bleeding), and iliopsoas muscle bleeds are known to be a muscle at risk of bleeding.
Monitor for femoral nerve palsy
A bleed into the iliopsoas muscle may not be easily recognizable

SIGNS AND SYMPTOMS OF AN ILIOPSOAS BLEED
Pain in thigh, hip, groin, abdomen or lower back
Unable to stand straight, or lie flat
Hip remains flexed
Inability to walk
Unable to sit up without pain
Numbness/tingling sensation along thigh.
Iliopsoas bleeds may occur due to an injury,
Psoas And Sacroiliac Joint
the psoas major can also potentially affect the sacroiliac joints in another way.
When it contracts, the psoas major creates a pulling force toward both the proximal spinal attachments and the distal femoral attachment.
If both attachments are stabilized, and therefore do not move, the psoas major would create a “bowstringing” force upon the pelvis that “pushes” it in the posterior direction
This force would certainly translate into and have an effect upon pelvis posture generally as well as specifically upon the sacroiliac joints.
Results A Sacroiliac Joint Dysfunction
Joint Bleeding
The knees, ankles, and elbows are more commonly affected by hemophilic bleeding than other joints.
This is attributed to two main reasons.
First, these joints have one degree of freedom of movement — as simple hinge joints,
Second, the hinge joints are not surrounded by protective muscles, whereas the hip and shoulder joints are covered by many layers of strong muscles.
Avoid aggressive exercise too early
Monitor for nerve compression
Use of heat modalities including ultrasound with precautions
No return to sports or activity until pain-free full ROM and strength
Postural Considerations in Bleeding disorders
People with hemophilia who have had many bleeds tend to develop a distinctive posture that may include:
flexion deformities of the elbows, knees, and hips;
an exaggerated arch in the back (lumbar lordosis);
plantarflexed ankles;
pelvic asymmetry due to leg length differences;
Flexed wrist and fingers caused by deep forearm bleeds are less common
A distinctive posture develops in predictable patterns according to the positions that joints and muscles prefer when there is a bleed in the area.
Unless there is a conscientious and sustained attempt to restore full joint motion, muscle flexibility, and muscle strength, this posture can become typical for the individual and the weak muscles continue to weaken and the tight muscles become even tighter.
Hemophilic arthropathy:
In an early stage of arthropathy, osteochondral damage is probably the result of the direct effect of blood and iron on chondrocytes. Blood is toxic to human cartilage after only 2 days12 because the formation of hemosiderin and hydroxyl radicals leads to chondrocyte apoptosis and impaired renewal of the extracellular matrix. The growing cartilage of children is more susceptible to this kind of damage.
Around 50% of patients with hemophilia will develop severe arthropathy.
Symptoms
Pain
Swelling
Temperature Variations
Limitations of movements
Pain during getting up from the chair
Pain during stair climbing
Joint Deformity
Repeated episodes of hemarthrosis lead to joint remodelling and subsequent hemophilic arthropathy, the targets of which are the diarthrodial (synovial) joints (i.e., freely moving joints whose surfaces are covered by hyaline articular cartilage that interfaces with a film of viscous fluid secreted by the synovial membrane).
This synovial fluid lines the joint capsule and consists of macrophage‐ and fibroblast‐like synoviocytes that normally form a few layers on the subintima with no basal membrane.
A first episode of hemarthrosis typically occurs in hemophilic children after the age of 1 year, and mainly depends on the severity of the factor deficiency. The bleeding mainly affects large joints such as the knees, elbows, or ankles, with the weight‐bearing joints of the dominant side being frequently affected as children begin to walk.
Repeated hemarthroses are responsible for the development of synovial hyperplasia and angiogenesis, with further bleeding occurring in the friable and thickened synovium.
There is evidence that even a single episode of hemarthrosis can start the inflammatory process that leads to synovial thickening and irreversible angiogenesis, thus predisposing to recurrent bleeding.
Soft‐tissue swelling and effusions are rare, and joint contracture occurs from muscle retraction and bone ankylosis, particularly if the muscles are weak. The level of pain varies and fluctuates, but may be severe.
The cartilage is progressively damaged by iron deposition and lysosomal enzymes and pro‐inflammatory cytokines produced by the inflamed synovium, which eventually leads to subarticular bone cyst formation.
Haemarthropathy will show features of both Rheumatoid arthritis and Osteoarthritis.
In more advanced stages, the joint is grossly damaged by cartilage loss and subchondral bone sclerosis, which further limits movement and leads to crepitus and deformity.
Physically active children are at higher risk of developing arthropathy, but regular physiotherapy and physical activity reduces the recurrence of joint bleeding by promoting joint stability. Early rehabilitation is strongly encouraged after the resolution of an acute episode of hemarthrosis
In chronic stages incidence of deformities are common
Arnold-Hilgartner classification is a plain radiograph grading system for haemophilic arthropathy of the knee
stage 0: normal joint
stage I: no skeletal abnormalities, soft-tissue swelling is present
stage II: osteoporosis and overgrowth of the epiphysis, no cysts, no narrowing of the cartilage space
stage III: early subchondral bone cysts, squaring of the patella, widened notch of the distal femur or humerus, preservation of the cartilage space
stage IV: findings of stage III, but more advanced; narrowed cartilage space
stage V: fibrous joint contractures, loss of the joint cartilage space, extensive enlargement of the epiphyses with substantial disorganization of the joint
Ligament Laxity
Joint bleeding stretches the joint capsule and ligaments and leads to joint instability, which is worsened because reduced joint motility from pain causes peri‐articular muscle weakness.
The physiotherapy techniques should be aimed to improve the muscle strengthening programs to compensate laxity.
Consider the chance of bleeding while planning any resisted exercise programes
Prepared By
Dr.Gayathri Rajeevan (PT)
BPT,MPT (Cardio Respiratory)
Senior specialist physiotherapist at rebounds physiotherapy and rehabilitation center





Comments